Medical and Pharmacy Benefits Management Application
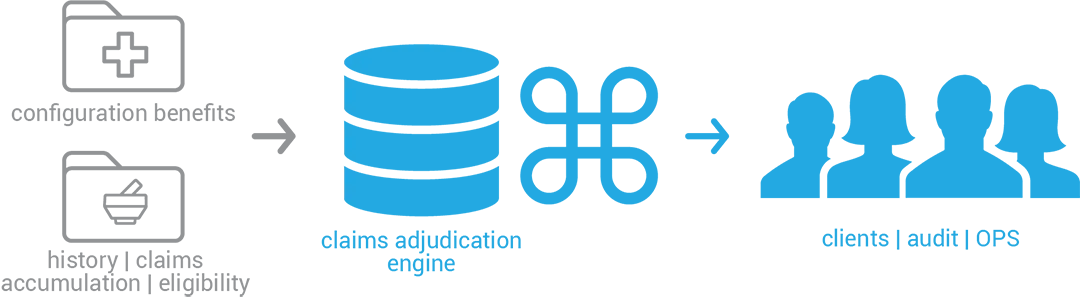
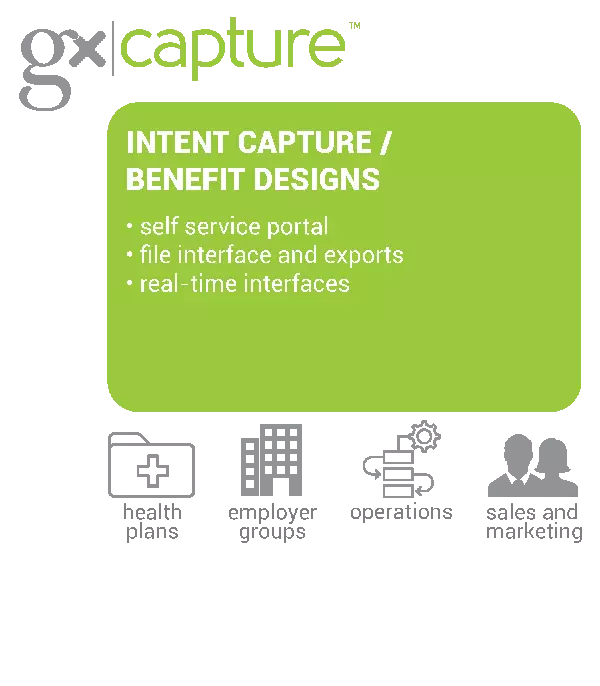
GxCare® is an automated benefits plan management system for benefit intake, modeling and cataloging that provides clients simplified benefits access for easier benefits maintenance and complete traceability. Automated benefit certification and benefit reuse are just some of the advantages that will drive increased operations efficiency, accuracy and enhanced speed to market. Designed to be scalable and flexible with rules-driven translations and benefit loading, GxCare® traceability means you are always audit-ready.
%
increase in efficiency through the use of automation
%
reduction in errors, decreasing performance penalties
%
reduction in production errors
Globally Implemented at Fortune 20 Organizations
blank
Distinctive Features
- Complete codebase for RxClaim and variants, and those of other top PBMs
- Documentation: process handbook, training material, marketing collateral engagement and deployment model
- Record type library & maps into specific adjudication engine
Invention
- Record type repository and dictionary (>400 record types)
- Modeling using historical claims (using GxClaims®)
Asset
- Complete codebase for RxClaim and variants, and those of other top PBMs
- Documentation: process handbook, training material, marketing collateral, engagement and deployment model
- Record type library & maps into specific adjudication engines
Scale Opportunities
- Involves our client in their clients product development
- Documentation: process handbook, training material, marketing collateral, engagement, and deployment model
- Record type library & maps into specific adjudication engines
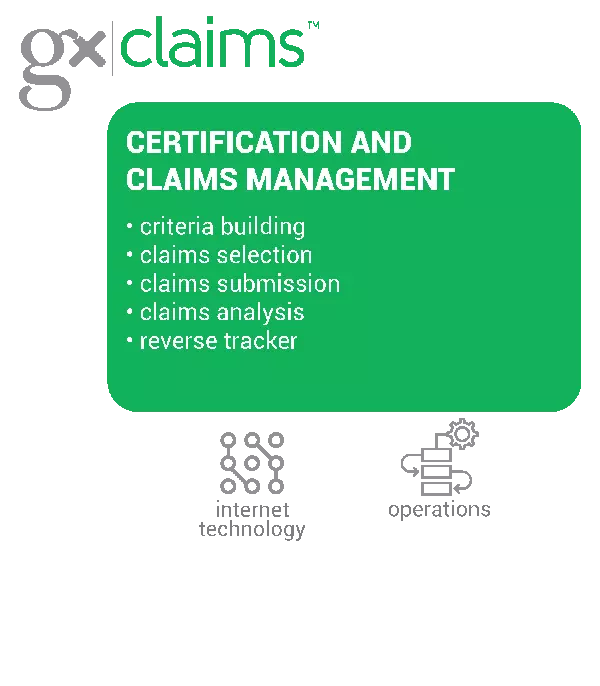
To unleash the full power of GxCare®,
use with GxCapture™ (intent capture) and GxClaims® (claims verification).
use with GxCapture™ (intent capture) and GxClaims® (claims verification).


 Increase Member and Group Retention and Satisfaction Learn how GalaxE provides end-to-end support for the transition of business and technical operations for Payers migrating to READ MORE
Increase Member and Group Retention and Satisfaction Learn how GalaxE provides end-to-end support for the transition of business and technical operations for Payers migrating to READ MORE Gx Podcast 02: The Changing Landscape of the PBM Industry GalaxE's Chief Automation Officer and EVP, Dheeraj Misra, and VP Business of Development, Tore Carlson, discuss mergers and acquisitions, pairing up of health plans and PBMs and more. READ MORE
Gx Podcast 02: The Changing Landscape of the PBM Industry GalaxE's Chief Automation Officer and EVP, Dheeraj Misra, and VP Business of Development, Tore Carlson, discuss mergers and acquisitions, pairing up of health plans and PBMs and more. READ MORE Welcome to the GalaxE A brief introduction to our services and Gx products. Our offerings give the insight you need to recognize, prepare and deploy your data and transform your business for competitive advantage in the future. READ MORE
Welcome to the GalaxE A brief introduction to our services and Gx products. Our offerings give the insight you need to recognize, prepare and deploy your data and transform your business for competitive advantage in the future. READ MORE How End-to-End Management Can Benefit Your Business Managing benefit plans is time-consuming and subject to human error, which can affect performance and regulatory compliance. A firm alignment between business and IT leads to efficient benefits plan management. READ MORE
How End-to-End Management Can Benefit Your Business Managing benefit plans is time-consuming and subject to human error, which can affect performance and regulatory compliance. A firm alignment between business and IT leads to efficient benefits plan management. READ MORE The Future of Artificial Intelligence (AI) A look at what Artificial Intelligence might be in 2025 READ MORE
The Future of Artificial Intelligence (AI) A look at what Artificial Intelligence might be in 2025 READ MORE Work smarter with an integrated benefits management system Managing benefit plans is time-consuming and subject to human error, which can affect performance and regulatory compliance. A firm alignment between business and IT leads to efficient benefits plan management. READ MORE
Work smarter with an integrated benefits management system Managing benefit plans is time-consuming and subject to human error, which can affect performance and regulatory compliance. A firm alignment between business and IT leads to efficient benefits plan management. READ MORE Gx General Overview Our business-enabling transformations impact people, communities and industries throughout the U.S. and around the world. As a recognized technology innovator with Fortune 500 companies, GalaxE is responsible for the growth and success of many industries. READ MORE
Gx General Overview Our business-enabling transformations impact people, communities and industries throughout the U.S. and around the world. As a recognized technology innovator with Fortune 500 companies, GalaxE is responsible for the growth and success of many industries. READ MORE Infrastructure Health Check GalaxE infrastructure health check encompasses your entire network and provides you with a single source of truth on the health of your network systems. This current state network ‘snapshot’ and third party validation of all servers, systems and network appliances, can work as a guiding principle, industry benchmark, and road map to ensure you are… READ MORE
Infrastructure Health Check GalaxE infrastructure health check encompasses your entire network and provides you with a single source of truth on the health of your network systems. This current state network ‘snapshot’ and third party validation of all servers, systems and network appliances, can work as a guiding principle, industry benchmark, and road map to ensure you are… READ MORE GxClaims™ Brochure GxClaims™ is a demographic and clinical selection, benefit plan certification, claim adjudication analysis, and integrated defect tracking process designed to validate claims processing behavior and increase efficiency in identifying root cause for unexpected claims adjudication outcomes. READ MORE
GxClaims™ Brochure GxClaims™ is a demographic and clinical selection, benefit plan certification, claim adjudication analysis, and integrated defect tracking process designed to validate claims processing behavior and increase efficiency in identifying root cause for unexpected claims adjudication outcomes. READ MORE Increase Member and Group Retention and Satisfaction Learn how GalaxE provides end-to-end support for the transition of business and technical operations for Payers migrating to READ MORE
Increase Member and Group Retention and Satisfaction Learn how GalaxE provides end-to-end support for the transition of business and technical operations for Payers migrating to READ MORE Next Generation Brings New Technology Take a closer look at a few key important trends in the industry such as AI and Machine Learning, QA Automation, CI/CD, DevOps, and Blockchain Integration, and how these trends are steadily driving us toward a shared goal – faster and more transparent business. READ MORE
Next Generation Brings New Technology Take a closer look at a few key important trends in the industry such as AI and Machine Learning, QA Automation, CI/CD, DevOps, and Blockchain Integration, and how these trends are steadily driving us toward a shared goal – faster and more transparent business. READ MORE Welcome to the GalaxE A brief introduction to our services and Gx products. Our offerings give the insight you need to recognize, prepare and deploy your data and transform your business for competitive advantage in the future. READ MORE
Welcome to the GalaxE A brief introduction to our services and Gx products. Our offerings give the insight you need to recognize, prepare and deploy your data and transform your business for competitive advantage in the future. READ MORE How End-to-End Management Can Benefit Your Business Managing benefit plans is time-consuming and subject to human error, which can affect performance and regulatory compliance. A firm alignment between business and IT leads to efficient benefits plan management. READ MORE
How End-to-End Management Can Benefit Your Business Managing benefit plans is time-consuming and subject to human error, which can affect performance and regulatory compliance. A firm alignment between business and IT leads to efficient benefits plan management. READ MORE Work smarter with an integrated benefits management system Managing benefit plans is time-consuming and subject to human error, which can affect performance and regulatory compliance. A firm alignment between business and IT leads to efficient benefits plan management. READ MORE
Work smarter with an integrated benefits management system Managing benefit plans is time-consuming and subject to human error, which can affect performance and regulatory compliance. A firm alignment between business and IT leads to efficient benefits plan management. READ MORE